Usually, there is no obvious cause of a hernia. Sometimes they occur with heavy lifting. Hernias may be present at birth, but the bulging may not be noticeable until later in life. Some patients may have a family history of hernias. Any activity or medical problem that increases pressure on the abdominal wall tissue and muscles may lead to a hernia, including:
· Chronic constipation, straining to have bowel movements
· Chronic cough
· Cystic fibrosis
· Enlarged prostate, straining to urinate
· Extra weight
· Heavy lifting
· Undescended testicles
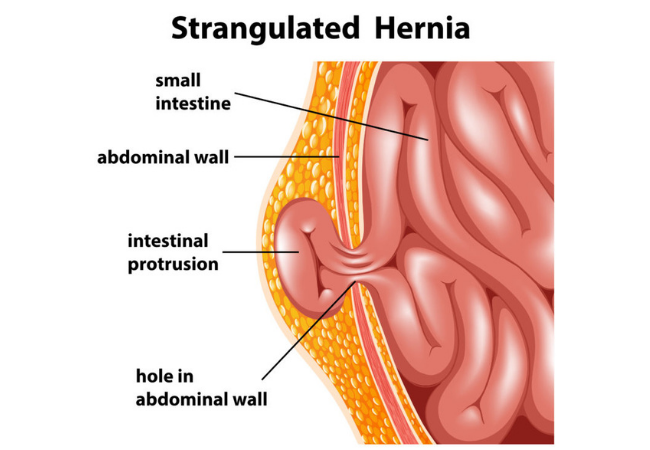
The signs and symptoms of a hernia can range from noticing a painless lump to the painful, tender, swollen protrusion of tissue that you are unable to push back into the abdomen. The most common symptom of a hernia is a bulge or lump in the affected area.
In the case of an inguinal hernia, you may notice a lump on either side of your pubic bone where your groin and thigh meet. You’re more likely to feel your hernia through touch when you’re standing up. Pain or discomfort in the affected area (usually the lower abdomen), especially when bending over, coughing or lifting. Weakness, pressure, or a feeling of heaviness in the abdomen a burning, gurgling, or aching sensation at the site of the bulge.
In case of anterior abdominal wall or incision hernia – mild discomfort in the abdominal area, pain in the abdomen outward bulging of skin or tissues in the abdominal area, nausea, and vomiting are common symptoms.
A doctor can confirm the presence of a hernia during a physical examination. The mass may increase in size when coughing, bending, lifting, or straining. A hernia (bulge) may not be obvious in infants and children, except when the child is crying or coughing.
Radiological modalities used are:
· Ultrasound of the abdomen area of interest
· Computerized tomography (CT) scan
· Magnetic resonance imaging (MRI)
If your hernia is growing larger or causing pain, your doctor may decide that it’s best to operate. Options for surgical treatment include:
· Mesh placement surgery:A surgeon pushes tissue back into place and then sews in a wire mesh (like a reinforcing patch) to keep it in place. This is considered safe and reliable.
Laparoscopic repair: A surgeon makes multiple small openings and fixes a mesh using a small camera inside the body to direct the surgery.
· Open surgery (non-laparoscopic). A surgeon makes a large opening and enters the body to push the tissue back into place and then sew it, reinforcing it with a mesh.
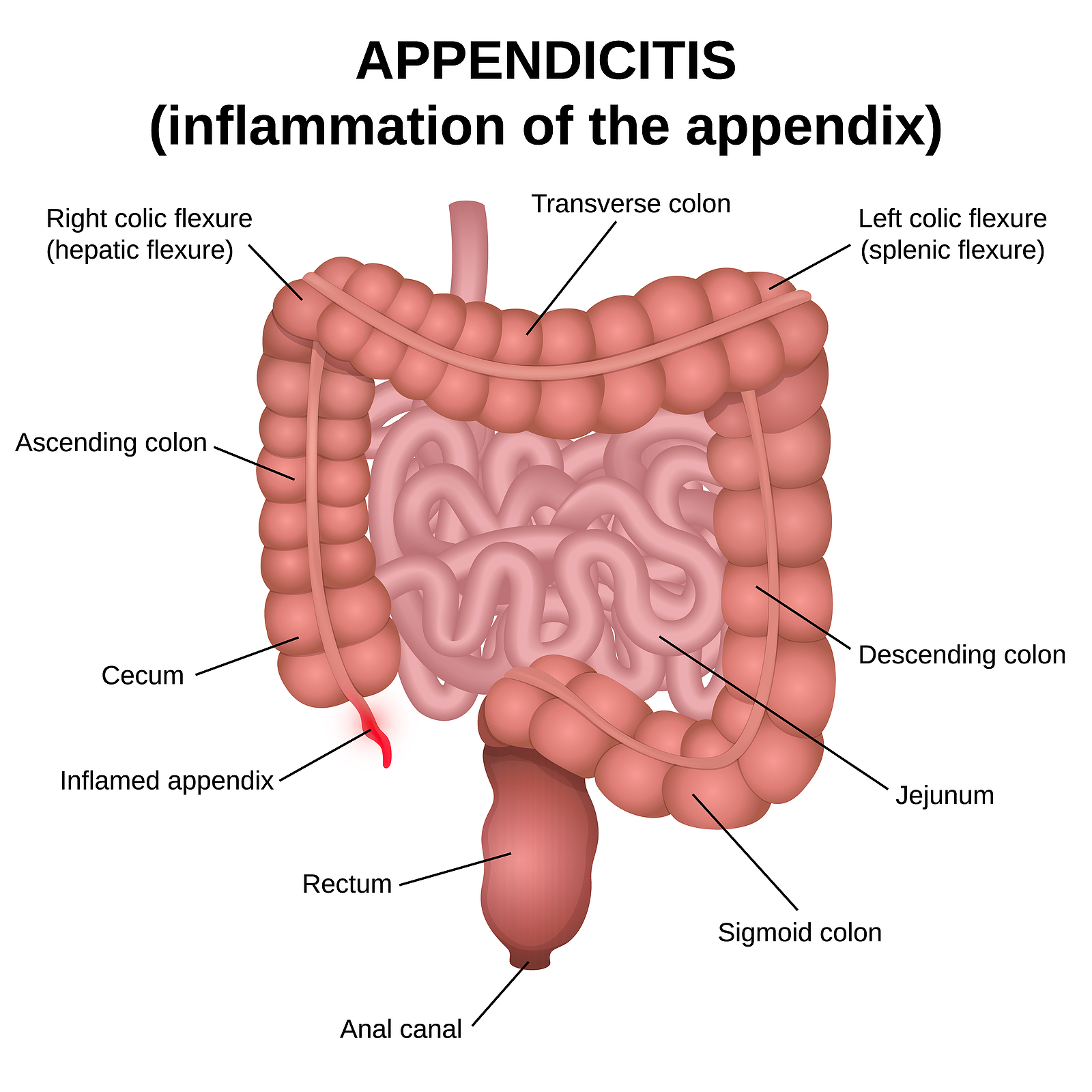
Symptoms are listed below.
· The best treatment of appendicitis is surgical removal. Mild appendicitis may sometimes be cured with antibiotics. More serious cases are treated with surgery to remove the appendix, called an appendectomy. Doctors either use an “open” technique or a minimally invasive approach to remove the appendix.
· Appendicitis is considered an emergency and anyone with symptoms needs to see a doctor immediately!
The laparoscopic (minimally invasive) surgical technique involves making several tiny cuts in the abdomen and inserting a miniature camera and surgical instruments. As many as three or four incisions are made. The surgeon then removes the appendix with the instruments, so there is usually no need to make a large incision in the abdomen. The camera projects a magnified image of the area onto a television monitor which helps guide the surgeons as they remove the appendix.
In a small number of patients the laparoscopic method is not feasible because of the inability to visualize or handle the organs effectively. When the surgeon feels that it is safest to convert the laparoscopic procedure to an open one, this is not a complication, but rather sound surgical judgment. Factors that may increase the possibility of converting to the “open” procedure may include:
· Extensive infection and/or abscess
· A perforated appendix
· Obesity
· A history of prior abdominal surgery causing dense scar tissue
· Inability to visualize organs
· Bleeding problems during the operation
The decision to perform the open procedure is a judgment decision made by your surgeon either before or during the actual operation. The decision to convert to an open procedure is strictly based on patient safety
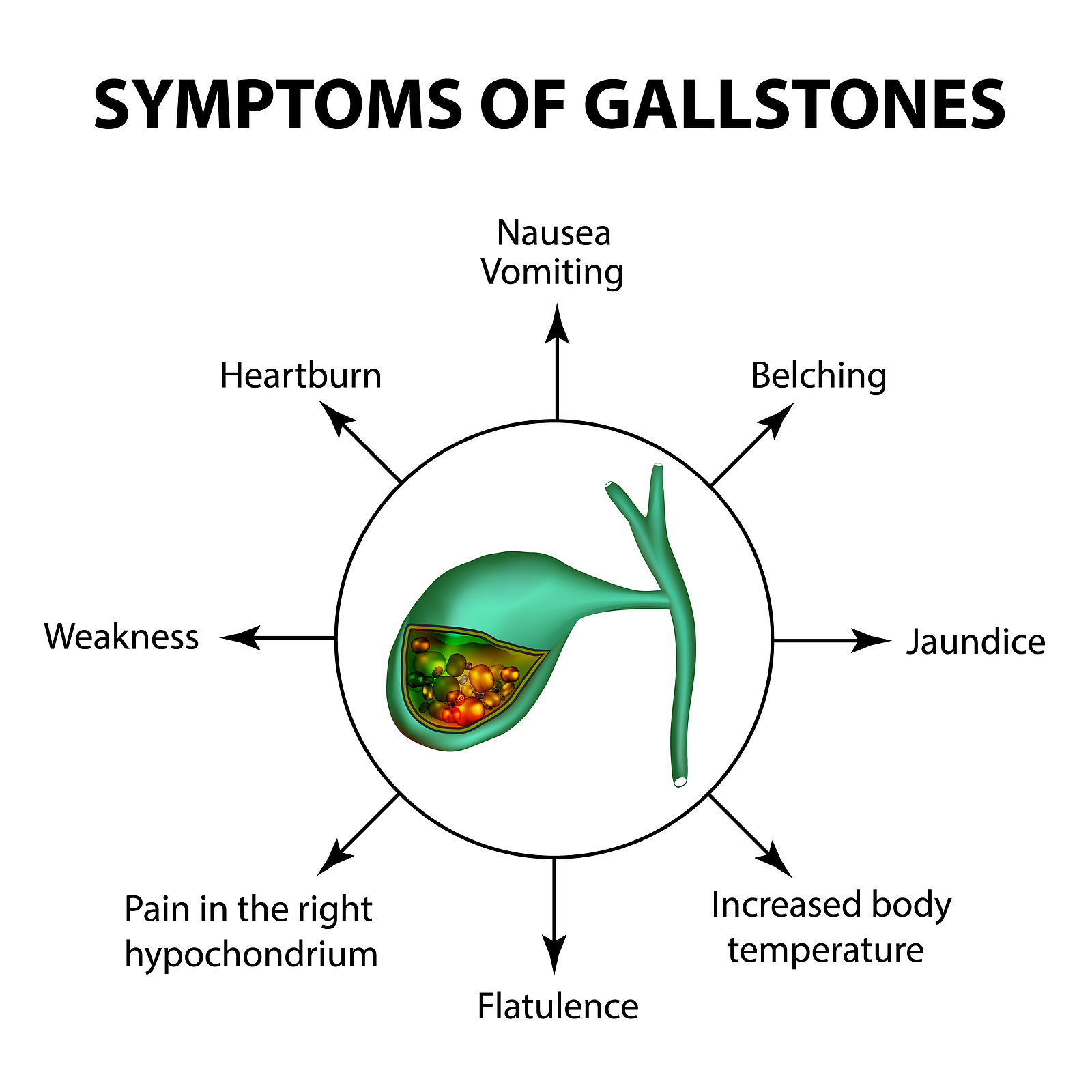
The presence of gallstones can be a strong cause for gallbladder problems. Excessive cholesterol in bile could cause gallstones. However, it is not very clear as to why gallstone forms in some people. There are no known cures for preventing gallstone. When this gallstone blocks the bile duct, it can cause jaundice.
Gallstones are usually diagnosed with the help of ultrasound. In other complex cases, x-ray may be taken to evaluate the severity of gallbladder disease. Gallstones do not disappear naturally. While some can be managed temporarily with drugs, the others are prevented by dietary adjustments like reducing the intake of fat. However, the success rate is very short-termed and low as well.
Cholecystectomy is the surgical removal of the gallbladder. It is a common treatment of symptomatic gallstones and other gallbladder conditions. Surgical options include the standard procedure, called laparoscopic cholecystectomy, and an older, more invasive procedure, called open cholecystectomy.
Laparoscopic cholecystectomy requires several (usually 4) small incisions in the abdomen to allow the insertion of operating ports, small cylindrical tubes approximately 5 to 10 mm in diameter, through which surgical instruments and a video camera are placed into the abdominal cavity. The camera illuminates the surgical field and sends a magnified image from inside the body to a video monitor, giving the surgeon a close-up view of the organs and tissues. The surgeon watches the monitor and performs the operation by manipulating the surgical instruments through the operating ports.
Being a major operation associated with the abdomen, there are chances for a certain amount of prospective pain. There could be an occurrence of vomiting and nausea. After the diet or liquid is tolerated, the patient can exit the hospital on the same day or the day after. Other activities largely depend on the patient’s feeling. Patients are encouraged to walk and showering is also allowed, a day after the operation.
A week’s time should be the ideal time for patient’s return to normal life. Things like driving, lifting of light objects, walking up stairs can be followed after that. One must understand the process of recovery is slow.
You must also understand that there are chances for complications. If you experience symptoms like yellow skin or eyes, fever or pain in the abdomen drainage or vomiting problems, contact your surgeon immediately.
