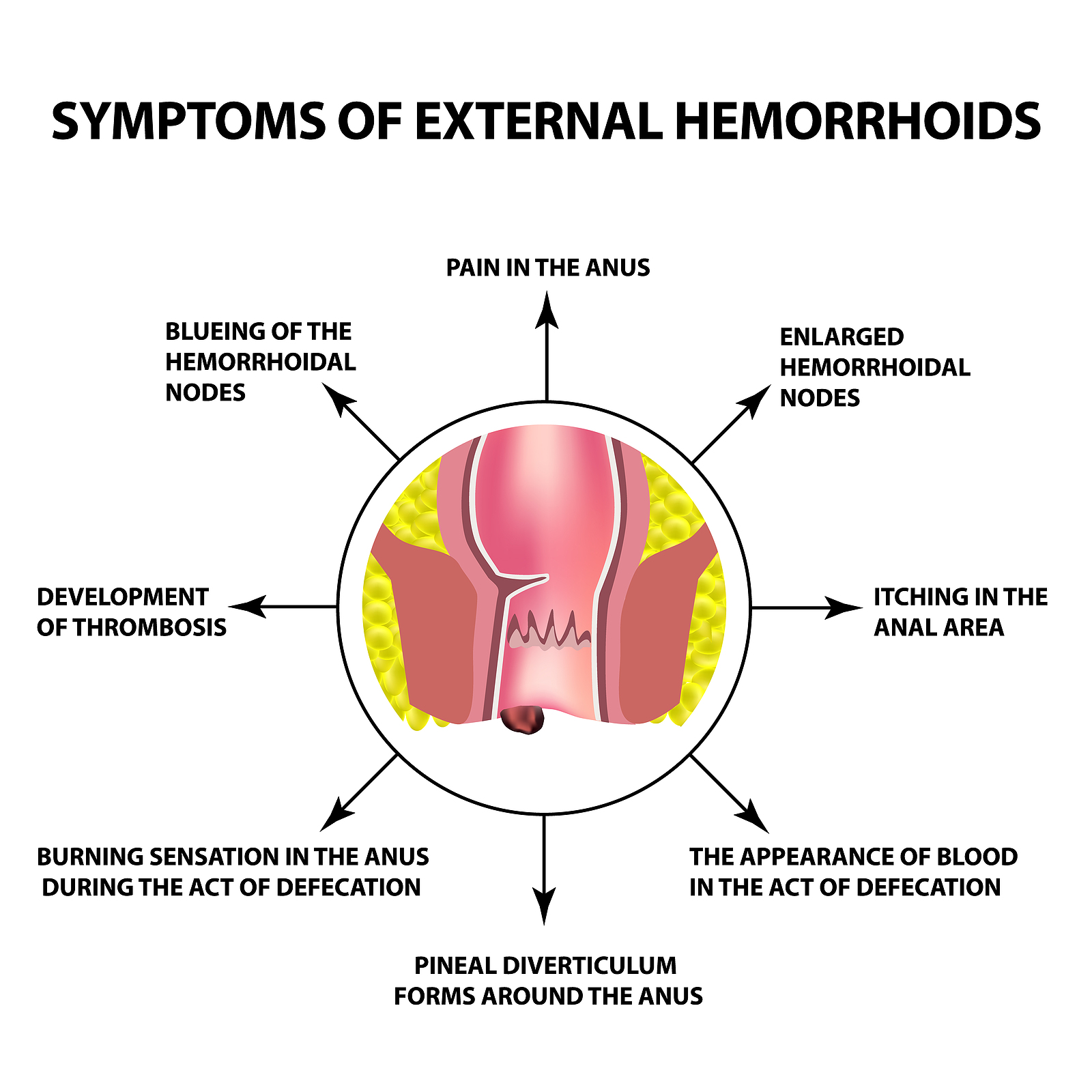


Piles are swollen blood vessels in the anal area, which can cause pain, itching, and bleeding. They can be treated with medications, lifestyle changes, or surgery.
A fistula is an abnormal connection between the anal canal and the skin near the anus, often caused by infection. Surgery is needed to treat it.
Laser treatment has revolutionized the management of conditions such as piles, fissures, and fistulas. Its minimally invasive nature, precision, decreased pain, minimal bleeding, prompt healing, and decreased chances of complications make it a compelling alternative to traditional surgery.
Dr Sanjitha Shampur is an expert in both, Laser and traditional surgical procedures.
Anorectal surgeries are commonly done using minimally invasive techniques, including lasers or laparoscopic methods, to reduce pain and recovery time.
A pilonidal sinus is a small tunnel under the skin near the tailbone that can become infected. Surgery is usually required to remove the sinus.
While rare, some anorectal problems may recur if the underlying condition is not fully treated. Proper care and hygiene are important post-surgery.
Recovery time can vary from 1-4 weeks, depending on the type of surgery performed and the patient’s overall health.
Dr.Sanjitha is very helpful and polite she responds very quickly to any issues related and I had got operated and was healed very quickly nice hand thank u mam fr all ur co operation 😊👌
She is a very kind doctor who listens to your issues and queries and Informs you of the options available to you in detail. She is available for any questions we can have and it is highly appreciated. she is willing to spend time to explain the procedures as well as comfort the patient. Duly recommend her services.
Very good doctor, she helped me with my problem which I didn't know what it was - I went to ortho doctor thinking some spine issue but madam told it's pilonidal sinus and did surgery for me. Now I am back to normal and painfree. Thankyou madam.
Dr Sanjitha was kind and approachable throughout the process of my treatment ... be it consultation , pre /post op check ups and follow ups . Thankyou mam . Please keep up your good work and continue to inspire all your fellow doctors.
Appreciate the thoroughness of the examination. Dr.Sanjitha took the time to explain everything in detail. I want to express my heartfelt gratitude for your unwavering dedication and compassionate care. Thank you for being an exceptional doctor.
Dr.Sanjita is very kind and an energy booster, I would say. She always give a positive energy and we don't even feel like we are sick, and responds immediately even for messages. I have done hemorrhoid surgery recently. I was totally scared to go to a doctor and do the surgery. But from the first consultation itself I got a very good confidence from the way doctor treated me and explained the procedure. I would really recommend her. Thank you Doctor 🙏
Click Here to View Google Map

Website Designed by HappiMed